Few health professionals divide people quite like chiropractors. You might think they are either quacks, or geniuses, and have evidence that you think supports your opinion. But what do you know about the education of chiropractors?
How good is the knowledge of graduate chiropractors? Are their beliefs based on evidence? And what are some of the misconceptions that chiropractic students and graduates possess?
We’ll start with some background.
Why chiropractors?
Because their treatment is not without harm. A recent death at the hands of a chiropractor made news around the world, but it’s not an isolated incident. High speed manipulation of the cervical spine can result in, at worst, a coronary artery dissection, and stroke. Estimates of how likely this is vary from once in every 100 000 to two million adjustments, as these events don’t always occur immediately after the treatment. They result in death in 18% of cases.
Very few medical treatments are totally without risk, so this doesn’t mean we need to avoid this treatment completely. As an example, physiotherapists in New Zealand have a comprehensive code of practice that details the screening to be conducted before this treatment is used. So they make a calculated decision, assessing the risk against the benefit of the treatments. If the benefit is small, or no better than a placebo, then the risk we will accept is far less.
Origins of chiropractic education
Chiropractic has dubious origins. Daniel Palmer, a beekeeper and grocer who practiced various forms of alternative medicine on the side, is credited with creating the practice. He borrowed heavily from osteopathy (which has been developed about a decade earlier), and at one point considered establishing the practice as part of a religion.
Palmer made most of his money from chiropractic schools rather than treating patients, and many of these schools were considered diploma mills.
We’re not off to a great start, are we?
Daniel Palmer, the founder of chiropractic treatment and education
What did early chiropractors believe?
The origins of chiropractic thought come from a tradition called “vitalism”. This is the idea that living beings have a life force that makes them distinct from inanimate objects. We’ve never been able to show this exists, but it’s a common idea in alternative medicine.
Palmer proposed that misalignments in the spine disrupted the flow of this life force, and interfered with the body’s natural healing mechanisms. In chiropractic these are called “subluxations”.
Confusingly, in evidence-based practice subluxations are a dislocation of a joint, and are usually very obvious. But chiropractic subluxations have not been reliably demonstrated. They are usually assumed to be present because of the symptoms reported by the patient.
So to summarize, chiropractors used to believe in a mystical life force that allows us to heal ourselves. If we are sick, it must be because our spine is out of alignment, interfering with this life force. But we can’t observe this life force, or these subluxations.
I’m not convinced so far, but surely this is all in the past, right?
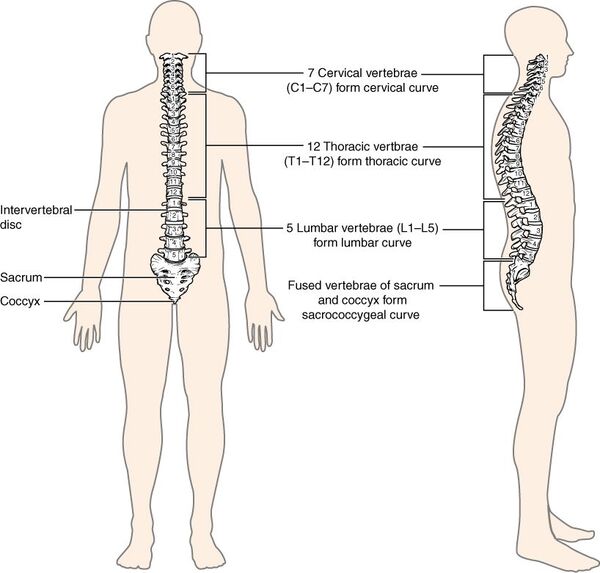
The spine. Apparently, the source of all disease. Source: OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/7-3-the-vertebral-column
The education of chiropractors today
Fast forward to today, and what has changed? For some chiropractors, almost nothing. For others, quite a bit!
There are now two general schools of chiropractic thought. Different degree qualifications will align more with one than the other, and this will influence what your chiropractor is taught.
Traditional chiropractic education
Those with a more traditional education will be more convinced that “subluxations” are the major cause of poor health. They are more likely to use x-ray as a diagnostic tool, even though subluxations are not visible on an x-ray. They are also more likely to have negative views about vaccination, and have more positive opinions about the effectiveness of their treatments.
Practitioners educated in this traditional approach may claim they can treat, or manage, a wide range of medical conditions (which we’ll discuss more below). After all, they’re highly confident that their practices are effective.
Modern chiropractic education
One university offers a chiropractic degree where I live, and it appears to have a modern approach. Their description of the role of chiropractors focuses on assessing and treating clients with back pain. They mention the importance of immunisation in protecting patients, evidence-based practice, and scientific reasoning skills.
Some researchers from this school have even done a good job of identifying the beliefs of chiropractic students that are not based on solid evidence.
Practitioners of this modern approach may use a range of treatments more consistent with modern physiotherapy, not just spinal manipulation. They may also be more conservative about what they can claim to treat.

Modern chiropractor’s don’t restrict themselves to spinal manipulation, but may provide specific advice about exercise and movement, and use a range of manual therapies as needed.
Chiropractors’ scope of practice
So chiropractors (in Australia at least) usually have five years of education, then may practice while claiming to treat a broad range of medical conditions. And they usually use the title of “Doctor”, which is unusual for not having completed a doctoral degree. So it’s understandable that there is some public confusion about the status of chiropractors as health professionals. But despite the title, without a lot of extra training, they do not complete anywhere near the training of a general practitioner, for example.
The scope of practice of chiropractors varies between countries, and even within countries. In the US it varies from state to state, but all include “providing care for musculoskeletal conditions using manipulation as a primary intervention“. And all states exclude the prescription of drugs, and surgery. But there is significant variation from one state to the next on other issues.
But what other treatments or advice they can provide, and what they are qualified to provide, is far murkier…
Even chiropractors can’t agree on their scope of practice
This schism in the industry begins with education (as discussed above). Of students surveyed in the US, 67% intended to sell nutritional supplements, and 46% to sell orthotics. And alarmingly, 80% thought they were qualified to diagnose disease. In another study 50% thought adjustments strengthened the immune system, and 72% thought adjustments “help the body function at 100% of its capacity.” Whatever that means.
It doesn’t end there. An alarming number of qualified, practising chiropractors agree that they can treat asthma (64%), gastrointenstinal complaints (61%), pre-menstrual stress (70%), osteoporosis (43%), hypertension (42%), and infertility (30%). Again, how likely a chiropractor is to hold these beliefs is influenced by where they were educated.

Physicians can diagnose, treat, and manage a range of medical conditions. Chiropractors cannot. They have many years of specialist training to enable them to do just that. Chiropractors do not.
You name it, some chiropractors think they can treat it. Not only do many of these beliefs lack evidence, they are implausible. With a decent knowledge of anatomy and physiology we can’t even come up with a decent, testable hypothesis to test how spinal adjustment could treat these issues.
And what proportion of chiropractors think they should restrict their practice to musculoskeletal issues? Alarmingly, just 6%.
This is staggering. I have never before seen an entire profession just decide to ignore the scope of their qualification. Oh, yes I have: personal trainers!
How did it get to this? Shouldn’t we know better?
You’d like to think that these sort of extravagant claims get ignored, but that’s often not the case. Chiropractors are extremely popular, as far as alternative health practices go.
It may be because people don’t really understand what chiropractic is. I’ll summarize again: a life force (that we can’t measure) keeping us healthy gets blocked by subluxations (that we can’t see) in the spine, and removing these will cure literally all disease. That’s traditional chiropractic thought in a sentence.
Our answer to a claim like this should always be “how do you know?”. If we’re relying on something we can’t see to treat something we can’t measure, we’re talking about something we can’t test. It’s literally impossible to prove that this treatment works.
Lots of alternative medical practices propose an innate life force of one kind or another. But we’re not aware of any genuine evidence for it yet.
Burden of proof
If you make a claim you have the burden of providing the proof for this. Would you let anyone else provide medical treatment without any proof that what they were doing was actually effective? If not, why would chiropractors get a pass?
A beautiful analogy for this was provided by Nobel Prize winner Bertrand Russell. It’s called (appropriately) “Russell’s Teapot”:
If I were to suggest that between the Earth and Mars there is a china teapot revolving about the sun in an elliptical orbit, nobody would be able to disprove my assertion provided I were careful to add that the teapot is too small to be revealed even by our most powerful telescopes.
Of course, we shouldn’t accept him at his word. He would need to prove this to us. Just like the medical treatments we consent to need to be founded on strong evidence.
Why do some chiropractors think this way?
Great question, but a difficult one to answer. How does a health professional get to the point where their beliefs are so at odds with the evidence?
The first issue is a lack of general critical thinking skills. Understanding where the burden of proof lies, and how to assess the quality of proof, is important. To the traditional chiropractor there is plenty of proof in the results their clients get – all anecdotal.
Which leads us to the second factor… bias. In any person it’s very hard to know why their pain gets better or worse, or why their symptoms change. Literally dozens of other factors influence our condition. And we usually attribute the change to whatever suits our biases. For chiropractors, that will often be their treatment, rather than the dozens of other factors we could consider.
Finally, we see a poor tolerance of uncertainty in many chiropractors. They aren’t alone here – many people find it hard to put things down to chance, and search for agency where none exists. That’s how conspiracy theories start. And why we tell ourselves that things happen “for a reason”.
This means that treatment can be uncertain, because not everything has a clear cause. In fact, back pain is a classic example of this. And sometimes in medicine a diagnosis is made only because we exclude everything else it could likely be.
This is intensely unsatisfying to some people. And often the more ignorant you are of these possibilities, the simpler the answer seems. It’s been my experience that once you appreciate the complexity of an area of knowledge you realise how hard it is to be definite. And the body is incredibly complex.
Models of healthcare
This lack of tolerance for uncertainty is made worse by the model of healthcare that persists among chiropractors, according to New Zealand physiotherapist Aaron Marshall:
Chiropractic care still lives within the biomedical paradigm. This is where a specific anatomical cause leads to specific symptoms. However, most medical and clinical professionals now appreciate the need for a biopsychosocial approach, where other factors contribute to the presence of pain or a syndrome.
We’ve discussed this before when examining the practices of physiotherapists. If your clinician is not open-minded enough to appreciate the complex, multi-faceted nature of pain, you may not be getting the most effective treatment.
Current chiropractic practice
By this point we’ve hopefully agreed that chiropractors can manage a range of musculoskeletal complaints, but should avoid more general health claims. But many don’t, because they did not learn the basics of scientific thinking in their qualifications.
Some modern chiropractors may not look that different from physiotherapists in their advice around exercise and load management, maybe with some manual therapy thrown in.
But we may see more high speed spinal manipulation, often for the management of back and neck pain. There is little evidence for the use of these manipulations for any other issue, but even with back pain, research is conflicted.
The gold standard of evidence – a Cochrane review – in 2011 found a mild, short-term benefit, that was about as effective as other treatments at the time. A more recent review in the British Medical Journal reached similar conclusions.
But an update to the Cochrane review identified that manipulations are no better than a placebo. And we even see similar results in chiropractic journals, so accusations of bias are hard to support.

Back pain is complex, and multifactorial. But research shows the benefits of spinal manipulation is limited, at best. Other approaches may be needed.
Chiropractors are more likely to treat when it’s not needed
For other health professionals, providing unneeded treatment is unethical. After all, some treatments come with a level of risk – and we’ve already identified there’s a risk from spinal manipulation. And all treatments cost money. So if there’s no benefit to the patient, we don’t provide the treatment.
In my professional experience, clients appreciate your honesty if you tell them they don’t need to see you. Or if you direct them to someone who could provide a more useful service. This is part of good professional practice. Clients like that you save them time and money, and may refer their friends to you. And other professionals appreciate the referrals, and may refer other people to you. Everyone wins – clients and practitioners.
Traditional chiropractors have a different approach. If your belief is that spinal manipulation can treat almost any condition, you will think everyone will benefit from seeing you at the slightest ache, pain, or runny nose. And given so many chiropractors see treatment as helping “the body function at 100% of its capacity”, they may see it as kind of like a tune up. Not compulsory, but certainly recommended. For the rest of your life!
So many are prepared to treat you, even if there is no obvious need. Physiotherapist Aaron Marshall thinks that “given the limited financial resources of most people, charging for a treatment that is not needed is something most clinicians should baulk at.”
Public perception of chiropractors
Despite flawed educations, claims that cannot be proven, a lack of scientific thinking, and unnecessary treatment being rife in the profession, chiropractors are generally viewed positively by the public. They also get generally positive discussion on social media.
And students obviously have a positive view of chiropractic treatment before they start studying. So they are exposed to public positive messages, and receive an education that fits their beliefs and values, which they choose because they want to help people. Their profession quickly becomes part of their identity.
And that’s ok, most of the time. But how would you react to evidence that your treatments are no better than a placebo, as we discussed earlier? Do you shrug, and get another job? Or do you double down, and look for weaker, confirming evidence you trust more?
To make change in the profession, maybe we need to change what we accept as members of the public, or part of a community of allied health professionals. If the shortcomings of traditional chiropractic care were better known, their public reputation may be different. And we would expect better from them, like we do from other health professionals.
Why do you hate chiropractors so much?
I don’t. I’ve met some wonderful, caring, friendly chiropractors. I’ve even received chiropractic treatment myself for relief of neck pain caused by a couple of decades of contact sport. But I didn’t notice any significant, lasting improvement.
Like all health professionals, chiropractors mean well, want the best for you, and genuinely want to help. But they need to have an awareness, like every other profession, of what they can do, and what others can do better. And they need to have an awareness of when to change. Aaron Marshall thinks this is confronting for any health professional:
The truth is, the first time you tell a patient that what you were doing is no longer supported by research, it is terrifying. You feel like your reputation is lost and your career over. But really, people appreciate your honesty and your drive to do better for them. While it is hard to let go of your biases, when you do this, and put the patient front and centre in your practice, your effectiveness and reputation will improve.
Summing Up
I’m not criticising people here – I’m criticising their ideas. If your idea about is too precious or fragile to be criticised, it probably isn’t a good idea, especially when our health is at stake.
Chiropractors have a huge disadvantage when misconceptions not only survive, but thrive, in their education. The most damning comment comes from a paper by Innes and colleagues, when they identified just how many unscientific beliefs their own students possessed. Their findings were “at odds with a curriculum which is intended to prepare them to be lifelong learners, and hence capable of delivering evidence-informed care.”
Do better chiropractors.
Updates
13/10/2020: we originally wrote that chiropractic degrees in Australia were either four or five years. On further investigation is seems the degree programs in Australia are all three year undergraduate degrees, followed by two year masters degrees.
3/1/2021: a new systematic review (looking at the use of chiropractic treatment in back pain) was brought to our attention, so we’ve updated the article and linked to this review. It was consistent with the previous research we discussed, so our conclusions did not change.
20/2/2021: we originally relied on a high estimate, when talking about how often adverse events occurred after chiropractic adjustments. We’ve adjusted this to represent the full range of estimates


Your information is grossly inaccurate and skewed and if you wish to belittle a profession I suggest you actually find the truths. Palmer College if Chiropractic is in itself a 4 year degree after a 4 year university pre-requisite study and have you looked at the comparative education between an MD and a DC? A doctor of chiropractic learns much more anatomy, physiology, diagnosis (twice as much) neurology (3 times as much) etc. We do not learn pharmacology because we treat the body naturally and our diagnosis teaching includes the entire body.
Your description is not only untrue but is offensive and shows clear prejudice. if you want to compare professions at least do it honestly. I know of many places where D.C.s and P.T’s work together as a team. I’m shocked at the list of clear blatant false information in this article.
Hi Susan, your point about the comparative volume of learning chiropractors and medical doctors undergo is addressed in my linked sources. And I don’t bring up Palmer College of Chiropractic at all. But if I’ve misinterpreted the evidence I’ve cited, or made any factual errors, please let me know and I can update the article.
You literally are wrong about almost everything. Where is there a 4year degree? DC is a doctorate licsensed by state and national requirements. Dangerous? Millions get adjusted daily and chiros pay about 1000 a year in malpractice. What does an MD pay? Who does insurance think is more dangerous. This was fiction with no basis in reality. I could name a dozen other false hoods. Where did you get your degree? Online?
You do raise one valid criticism here Michael – I state chiropractic is a four-to-five year degree, but it appears that the degree programs in Australia are all 5 year programs, so I’ll make that correction to the article.
Everything else in the article is informed by research. This includes the discussion of risk that you refer to in your comment. I don’t refer to chiropractic treatment as dangerous, but I do make the point that (like in all things) we need to assess risk against benefit. Even when that risk is low.
I’m always looking to make my articles more accurate, so if you identify any other specific errors (with appropriate evidence, of course), I’d be glad to update the article.
This is a paid hack job
Fake News
Lame
Hi David, this hack job did not earn me a cent (unless you clicked on an advertisement). It’s just a hobby.
As I’ve told every other chiropractor who’s been upset by this article, if you can let me know what specific errors I’ve made I can correct them.
It’s alarming that for health professionals, none of the chiropractors that have commented here have shown any desire to engage in analytical thinking.
As a profession you can’t improve if you’re not willing to critically examine your own practices and education.
hi! what i don’t like about chiropractors, it isn’t holistic anymore specially here in philippines. they make you as their cash cows, requiring you to keep coming back and selling packages of sessions. i’ve only encountered 1 german chiro who doesn’t keep you coming back, told me if there’s no pain don’t come back…
Hi Samuel, yes, that’s a complaint I’ve heard many times before. I think generally they believe they are helping that person with those continued visits, particularly when you think about some of the misconceptions we discuss in this article.
You obviously have not done your ‘criticai’ homework, thus research as a good Ph.D. should do! You have shown your biases, rather than done a true investigation!
Rather than break down and challenge each falsehood statement, which seems exhausting: I’ll just leave alon, let you go back do some fact checking on some of your statements, and resubmit this poorly written article- SHAMEFUL!
Louis Valencia, BSc, DC, CSCS
https://www.naturalhealers.com/chiropractic/degree/
You’ve probably noticed that I’ve provided sources throughout the article. If it seems exhausting to thoroughly critique a piece of writing, it should, because that takes time and effort – much like writing it in the first place. But I would take your criticism far more seriously.
Very informative and accurate article. The amount of comments from Chiropractors calling you a liar without providing any refuting evidence essentially proves your point. Most of them lack basic critical thinking and especially skills in critical analysis.
Thanks for reading Michael. I agree with your point here!
Thank you for writing this. I am a DC as well. This is anti Chiropractic propoganda. Must have some connection to a threatened physical therapist, osteopath, orthopedist, or physiatrist. It was clear reading this that he has never really learned about the profession in any depth. I have a license in Massachusetts/US. He is also still in the land of Newtonian physics with regards to the body. Does not know Dr Candace Pert, Dr Bruce Lipton, Dr Lynn Tagert, or Dr Joe Dispenza’s scientifically based books and understanding of health.
Hi Kate, thanks for reading.
You should note that I have also been critical of physical therapists on this site, though I’ve worked closely with many in the past. I’m also highly critical of fitness professionals where needed. After all, if we aren’t critical of our professional practices, how can we improve them? So your accusation of propaganda rings a little hollow. You shouldn’t be threatened by criticism, you should welcome it, and make sure your professional practices are sound enough to stand up to scrutiny.
You have minimal knowledge of our profession
We have staff privileges at many hospitals…ignorance and bias .
Shame you belong about 2o years ago..
If I’ve made any errors in the article, please let me know, I always strive to produce accurate work. But you’ve instead chosen to accuse me of being ignorant, biased, and out of date. What do you think a casual reader would think of a professional that chooses to make these accusations, rather than engage in a discussion of research and evidence?
I graduated from SCUHS for my D.C and I had to have a 4 year undergrad degree as a premed to get into the school. I did my B.S at UCLA in psychobiology. We got indepth education in chiropractic school, very similar to my MD friends except we had fewer classes of pharmacology. As primary physicians in CA we are also able to order blood work and help patients improve through life style as medicine. The holistic approach addresses the spine and overall health. We get way more hours compared to other professions in nutrition, and on top of that many of my colleagues did seminars to further their education. Chiropractic community helps so many people get better which is why most insurance companies pay for chiropractic treatments to keep their insured healthy. We are also able to specialize in a filled and pass a board exam to practice that specific area such as neurology, pediatric, radiology, nutrition or sports medicine.
Hospital-acquired infections, anesthesia mishaps, falls, and drug errors are the most common iatrogenic events and count for the third leading cause of death in USA after heart disease and cancer.
I honestly feel your article is biased and your writing is putting down the profession.
I believe in the innate intelligence concept. When an egg and sperm meet and those cells multiply beautifully to make a human, that is the working of innate intelligence within the cells. Do I have a research paper showing that with control groups? No, but I have studied the human body for a long time and I know of its intelligence. I hope youbgrt to feel yours so you could understand it.
You probably also don’t believe in what goes around, comes around. But I do, so I will also say it’s important that you don’t carry this karma of putting Chrios down because they actually help so many people have a better quality of life.
Thanks for taking the time to comment Tara. I intentionally made very little comment on the length or breadth of chiropractic education, as that has been covered elsewhere (I linked to my source, if you’d like to critique it). But as a response, it’s a logical fallacy known as an “appeal to authority”. Despite this education, chiropractors possess significant errors in knowledge, and a disregard for their scope of practice. This was the point of my article. The length of an education isn’t relevant if the knowledge retained from it is flawed.
“When an egg and sperm meet and those cells multiply beautifully to make a human, that is the working of innate intelligence within the cells” that is not innate intelligence. Sperm follow chemokines to meet the egg, and cell proliferation and differentiation has nothing to do with intelligence. Your lack of knowledge of extremely basic biology is astounding and proves the writers point.
I thought your article was well balanced. Early chiropractic practice was quite dubious (just like how MDs used to blood let to rid the body of bad humours), but research in the field has encouraged chiropractic treatment for various musculoskeletal problems over traditional medical practices (at least in the U.S.). There is definitely a divide in the profession, and personally, I believe that the traditional way,outlined in your article, is outdated, and is the biggest contributor to the negative connotation surrounding the profession.
Thanks for reading Mike! Let’s hope there’s a continued shift to more modern practices.
I totally agree. This article is skewed and grossly misrepresents chiropracty. While I agree that all chiropractors are not of like ability, this is the same in the medical profession or any other profession for that matter. I have certainly been helped by chiropracty for pains in my neck, back and shoulder. This is both a preventitive therapy and one that responds to acute events. Some chiropractors also study nutrition, as some medical doctors have a sub-specialty. Nutrition has been abandoned by the medical profession. This adoption of a competitive stance between medical doctors and chiropractors is stupid. It is no secret that the medical profession has abandoned preventative health and is now acting in general as purveyors of drugs to treat symptoms rather than root causes. When Medicine is treated like a business it views every other form of treatment as a competitor instead of another weapon against ill health and harm is done to the patient as a result. The Hippocratic Oath says “do no harm.” Stop the hypocrisy and practice real medicine. Chiropracty is a useful tool and works within its scope.
Hi Diana, as I offer to anyone criticizing this article, I will gladly update it if you identify any specific errors. But most of your comments aren’t related to the topic of the article, so you’ll excuse me for not making any changes just yet.
I think the biggest issue with our profession is the lack of funding for research. Many other medical professions have an astronomical amount of money and resources to use for research, where as chiropractic does not. I really believe that is why the chiropractic research is not able to substantiate many of its claims. For now, what we are able to go off of are anecdotal claims. And considering that a large amount of prescribed drugs “work” but the mechanism of how they work is unknown, I think that these anecdotal claims are enough for now. Just because we don’t know how something works, doesn’t mean it doesn’t.
There’s plenty of research into chiropractic practices. I cite it throughout this article.
In fact, one of your colleagues cites dozens of academic references in another comment to this post.
Great article, and every point you made is all backed up by endless studies, that proves that the field of chiropractic is more pseudoscience then anything else.
Sadly this knowledge is not aware in the general public.. that’s probably why the field is still so successful
Susan, your correct! But dont worry, this is simply a hack writer trying to stir up an audience to get more than 3 family members to read his stuff. He actually wants you to do his research to give him the correct info. No need for us to defend ourselves, our patients prove our worth everyday.
Hi Chris, you’ll note that I researched this article quite thoroughly. And I’ll gladly update the article to reflect changing evidence. But most of the chiropractors that comment here want to hurl insults instead. How do you think that makes you look to my readers?
Compared to PT school, getting into chiropractic schools is extremely easy since it’s not a competitive program, does not require any type of entrance exam, nor undergrad degree. Also, most schools have 90+% acceptance rate with gpa’s as low as 2.75/4. Chiro schools accept new students every semester. Compared to PT school which requires a high GRE score, undergrad degree, at least a 3.6/4 gpa to be considered and only accept 40 students per year (out of 1000-1500 applicants per school). PT and MD curriculums are extremely rigorous compared to chiropractic.
Can you provide citations that DC’s get 2x as much education in diagnostics and 3x in neurology (as M.D.’s do? you didn’t say).
You state that “Chiropractors are extremely popular, as far as alternative health practices go.” And then claim that this may be because people don’t understand what chiropractic is. Isn’t this just ignoring the obvious? Do you really think that millions of people are so stupid that they would routinely visit chiropractors and recommend chiropractic to their friends and families if they weren’t getting results? They are getting the results they are looking for. I’ve worked in a chiropractic office and been a chiropractic patient for over 30 years. In that time I’ve avoided seeing any medical doctors, avoided taking harmful drugs and being cut open. And yes, I do believe that keeping the nervous system free of interference allows the body to function at a higher level. That’s what people are looking for, and that is why chiropractic is so extremely popular.
Thanks for commenting Lynn. It’s great that you’ve had a good personal experience with chiropractors, and have been healthy and injury free for such a long time.
But the popularity of a treatment does not indicate that the treatment works. This is an example of an argument from popularity, and there are many others we could make too. Millions of people think 9/11 was an inside job, Barack Obama is a Muslim, or that COVID-19 is a hoax promoted by the New World Order.
Regardless, in this article when commenting on the effectiveness of chiropractic treatment, I’m referring to research to inform my conclusions. This type of evidence is more reliable than personal anecdotes. While this isn’t the focus of the piece, I’ll gladly update this section of the article if more research comes to my attention.
18 % death rate??? What are you talking about? More allopathic fiction. This type of professional discrimination was tried in the US years ago resulting in a victorious landmark lawsuit against virtually every professional medical association in the US. Upheld by the supreme court in 1991. Also review the study done in New Zealand years ago. Patients who get regular Chiropractic care have less strokes than those who are never adjusted. You very long article is profoundly disappointing
I’ve provided references for the figures I cite, but if you have more information feel free to point me in the right direction, and I can update the article accordingly.
Yes and 18% death rate OF the small subset that get injured. 18% of the 1 in 100,000 to 1 in 2 million injury rate… acknowledged as low, but present. You ignorant outrage is part of the problem here. You don’t ‘science’ well at all. And data is not discrimination, you poor picked on peevish man. A scam is a scam, and once scammed it is hard to believe one has in fact been scammed as often the sunk costs are too hard to mentally handle. <<- I just described your education. You're happy to make uncited claims, and troll for support like a wounded victim of the truth tellers instead of your own self sabotage.
This is an extremely biased article for anyone who has knowledge of Chiropractic. I’d say everything was presented in a poor and discrediting way. Chiropractic PHYSICIANS in the US go to school for about 8 years and they receive a Doctorate degree. Also the statistics used to estimate artery dissection rates are completely false.Most reputable sources agree this closer to 1 in every 2 million. Some even higher. In these cases it has not always been clear if to be considered a causation but rather an association. Blaming a Chiropractor for a patient with stroke 2 weeks after his visit is just unfair. There are too many factors to really pin down the source of his stroke. Also it is believed that some people may have genetic predisposition on the lining of their vessels. There is so much wrong with this article I could go on and on. Almost every point is wrong or twisted truth at best.
Chiropractic is safe. Chiropractic malpractice insurance is a fraction of that of a general medical practitioner. The insurance companies know the statistics so they charge very little in comparison.
There are multiple forms of Doctors. There are Doctors of Dentistry, Veterinarians, Doctors of Medicine and even Doctors of Chiropractic. When I visit my dentist, I call him Doctor. This is a simple concept, I’m not sure why some people refuse to get it. When I visit my Chiropractor, I call him Doctor as well. For anyone reading this make sure you get informed from a reputable sources. Maybe look into length of studies and curriculum in a Doctor of Chiropractic school to get an idea.
As a matter of fact Chiropractic students go through more anatomy than general practitioner medical doctors. They do NOT do pharmacology which is why they don’t prescribe you medications.
Hi Omar, thanks for reading. If you have some more up-to-date, evidence-based sources of information to correct any of the statements I’ve made, please let me know and I can update the article.
It’s all in the manner of just going to the curriculum of studies. Go-to Logan College of chiropractic or Canadian Memorial College of Chiropractic websites. Here you will see that the training is at least equal to or greater than medical training, especially when you are looking at the original Hippocratic Oath.
Dennis Pick, D.C.
Hi Dennis, I have linked to a source that compares medical and chiropractic training in the article, if you wanted to read more. It’s not really a focus of this article, so I touch on it only very briefly.
I refer back to my original complaint regarding the education of a chiropractor. However, here is another chiropractic college that reveals the superior training of Chiropractic physicians: Canadian Memorial College of Chiropractic.
After reading the curriculum, I rest my case.
You mentioned that one already Dennis, but again, that’s not really the focus of the article. The point is, despite how good you think the quality of chiropractic education is, significant misconceptions survive this education. We should strive to be better than this in all fields of learning.
Where to even start…your last comment, ” have linked to a source that compares medical and chiropractic training in the article, if you wanted to read more. It’s not really a focus of this article, so I touch on it only very briefly.” Well, the title of your very biased and factually erroneous article is “The education of chiropractors is not all it’s cracked up to be.” So, from the title it seems like that SHOULD be the focus of the article.
I’m not sure why there is a need to constantly compare DCs to MDs but get your facts straight if you insist on doing so. Looking at the education of chiropractors vs medical doctors education in hours:
Anatomy-physiology: DC 540, MD 508
Microbiology: DC 120, MD 114
Diagnosis and derm: DC 630, MD 324
Neurology: DC 320, MD 112
Orthopedics: DC 210, MD 156
(Source: https://www.google.com/url?sa=t&source=web&rct=j&url=https://biology.uni.edu/sites/default/files/chiropractic_education_vs_medical_education.pdf&ved=2ahUKEwieovHE6OvtAhVLuVkKHYqzCC0QFjABegQIHxAF&usg=AOvVaw2f3dRYIhoP60I-eIuDbc7d. OR https://pubmed.ncbi.nlm.nih.gov/9737032/
Moving on to the next topic. You seem to only want to accept double-blind placebo co trolled clinical trials as evidence that something works. Do you know in the medical industry they use something called “off label” prescriptions…? Meaning they are using a medication for something that wasn’t part of the trials for the drug. Do you know they also do exploratory surgery? No double-blind studies on that either.
As surgeon and health care researcher Atul Gawande observes, “Millions of people are receiving drugs that aren’t helping them, operations that aren’t going to make them better, and scans and tests that do nothing beneficial for them, and often cause harm.”
I will agree that those DCs that continue to follow DD Palmer and his “vitalism” approach may not have much evidence to back their claims but there is plenty of research available that chiropractic is helpful in treating many conditions. In fact, some insurance companies (who don’t really care about the health of their policyholders beyond premium payments) are requiring either a trial of chiropractic or PT before injections or surgery.
Also, let’s look at what evidence-based practice means…it is a conscientious, problem-solving approach to clinical practice that incorporates the best evidence from well-designed studies, patient values and preferences, and a clinician’s expertise in making decisions about a patient’s care. So, the “evidence” that you seek to prove/disprove chiropractic is viable is only one of three aspects of EBP. So, to your previous response to the comment above, “But the popularity of a treatment does not indicate that the treatment works.” except it does in a way as EBP includes clinician expertise and patient values and preferences.
Now, let’s look at some more evidence that chiropractic is effective for treating some conditions:
“Spinal manipulation is an effective option for migraine and cervicogenic headaches.” Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3716373/#:~:text=Spinal%20manipulation%20is%20an%20effective%20option%20for%20migraine%20and%20cervicogenic,inconclusive%20for%20tension-type%20headaches.&text=There%20is%20little%20information%20available,Bronfort%20et%20al%20is%20notable.
Clinical Outcomes
LOW BACK PAIN
• The Agency for Healthcare Research and Quality reviewed the current evidence on nonpharmacological LBP treatments and found that spinal manipulative therapy (SMT) is an
effective intervention for chronic LBP.
• A systematic review published in the Journal of the American Medical Association (AMA) studying the effectiveness of SMT for the treatment of acute LBP found that “SMT was associated with modest improvements in pain and function at up to 6 weeks, with transient minor musculoskeletal harms.”
• Research suggests that SMT plus home exercise with advice is more effective than receiving only home exercise with advice for patients with subacute and chronic back-related leg pain.
• Results of a 2013 randomized controlled trial suggests that 12 sessions of SMT for chronic LBP offer the best “dose.”
NECK PAIN
• In 2016, the Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders found
that mobilization, manipulation, and clinical massage are all effective interventions to manage
whiplash-associated disorders or neck pain and associated disorders. Electroacupuncture, strain-
counterstrain, relaxation massage, and some passive physical modalities were not found to be
effective.6
HEADACHE
• Manual therapy consisting of SMT, mobilization, soft-tissue therapy, or exercise is more
effective than medication in the short term and as effective as medication long-term for muscle
tension-type headaches.
7
• Cervicogenic headaches, which may include muscle tension type headaches, can be effectively
treated with SMT, mobilization, and exercise by reducing headache intensity and frequency.
8,9
• SMT may be as effective for Migraine headache treatment as prophylactic medication use.
10
GUIDELINES
• A guideline from the American College of Physicians recommends nondrug treatment including
SMT for acute or subacute LBP. For chronic LBP, nondrug treatment should also initially be
selected including interventions such as exercise, acupuncture, mindfulness-based stress
reduction, yoga, low-level laser therapy, cognitive behavioral therapy, and SMT.11
• A guideline for chiropractic care for LBP recommends a treatment schedule of 2-3x/week for 2-4
weeks for acute or subacute pain. For recurrent or flare-up episodes, 1-3x/week for 1-2 weeks.
For chronic pain, 1-3x/week for 2-4 weeks. Reevaluations should occur between 1-4 weeks,
depending on the stage of pain.12
• In a guideline for chiropractic care for neck pain, SMT is recommended in combination with
conservative treatments such as mobilization and exercise in both the short and long-term for
the acute stage. For chronic, SMT is recommended as a sole treatment option as well as in
combination with other conservative treatments in the short and long-term.13
• SMT is recommended for treating patients with cervicogenic and migraine headaches, according
to a guideline for chiropractic care for headache.14
Risks
• Most of the adverse events reported in studies of SMT include mild and transient symptoms
such as aggravation of complaints, radiating pain, stiffness, muscle spasm, and fatigue.3,15,16
• A 2016 systematic review of the literature on cervical artery dissection following SMT found no
causal link.17 These findings are consistent with previous studies which have concluded that
increased risks of VBA stroke associated with both chiropractic and primary care are likely due
to patients seeking care because they are experiencing symptoms of headache and neck pain
due to ongoing VBA dissection.18,19
• A review studying serious adverse events related to SMT in the low back concluded that any
recorded events are anecdotal in nature and causality has not been established
REFERENCES
1. Sackett DL. Evidence-based medicine. Spine (Phila Pa 1976). 1998;23:1085-1086.
2. Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al. Nonpharmacologic Therapies
for Low Back Pain: A Systematic Review for an American College of Physicians Clinical Practice
Guideline. Ann Intern Med. 2017;166:493-505.
3. Paige NM, Miake-Lye IM, Booth MS, Beroes JM, Mardian AS, Dougherty P, et al. Association of
Spinal Manipulative Therapy With Clinical Benefit and Harm for Acute Low Back Pain: Systematic
Review and Meta-analysis. JAMA. 2017;317:1451-1460.
4. Bronfort G, Hondras MA, Schulz CA, Evans RL, Long CR, Grimm R. Spinal manipulation and home
exercise with advice for subacute and chronic back-related leg pain: a trial with adaptive
allocation. Ann Intern Med. 2014;161:381-391.
5. Haas M, Vavrek D, Peterson D, Polissar N, Neradilek MB. Dose-response and efficacy of spinal
manipulation for care of chronic low back pain: a randomized controlled trial. Spine J. 2013.
6. Wong JJ, Shearer HM, Mior S, Jacobs C, Cote P, Randhawa K, et al. Are manual therapies, passive
physical modalities, or acupuncture effective for the management of patients with whiplash-
associated disorders or neck pain and associated disorders? An update of the Bone and Joint
Decade Task Force on Neck Pain and Its Associated Disorders by the OPTIMa collaboration. Spine
J. 2016;16:1598-1630.
7. Mesa-Jimenez JA, Lozano-Lopez C, Angulo-Diaz-Parreno S, Rodriguez-Fernandez AL, De-la-Hoz-
Aizpurua JL, Fernandez-de-Las-Penas C. Multimodal manual therapy vs. pharmacological care for
management of tension type headache: A meta-analysis of randomized trials. Cephalalgia.
2015;35:1323-1332.
8. Chaibi A, Russell MB. Manual therapies for cervicogenic headache: a systematic review. J
Headache Pain. 2012;13:351-359.
9. Racicki S, Gerwin S, Diclaudio S, Reinmann S, Donaldson M. Conservative physical therapy
management for the treatment of cervicogenic headache: a systematic review. J Man Manip Ther.
2013;21:113-124.
10. Chaibi A, Tuchin PJ, Russell MB. Manual therapies for migraine: a systematic review. J Headache
Pain. 2011;12:127-133.
Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive Treatments for Acute, Subacute, and
Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann
Intern Med. 2017;166:514-530.
12. Globe G, Farabaugh RJ, Hawk C, Morris CE, Baker G, Whalen WM, et al. Clinical Practice Guideline:
Chiropractic Care for Low Back Pain. J Manipulative Physiol Ther. 2016;39:1-22.
13. Bryans R, Decina P, Descarreaux M, Duranleau M, Marcoux H, Potter B. Evidence-based guidelines
for the chiropractic treatment of adults with neck pain. J Manipulative Physiol Ther. 2014;37.
14. Bryans R, Descarreaux M, Duranleau M, Marcoux H, Potter B, Ruegg R, et al. Evidence-based
guidelines for the chiropractic treatment of adults with headache. J Manipulative Physiol Ther.
2011;34:274-289.
15. Rubinstein SM. Adverse events following chiropractic care for subjects with neck or low-back pain:
do the benefits outweigh the risks? J Manipulative Physiol Ther. 2008;31:461-464.
16. Walker BF, Hebert JJ, Stomski NJ, Clarke BR, Bowden RS, Losco B. Outcomes of usual chiropractic.
The OUCH randomized controlled trial of adverse events. Spine (Phila Pa 1976). 2013;38.
17. Church EW, Sieg EP, Zalatimo O, Hussain NS, Glantz M, Harbaugh RE. Systematic Review and Meta-
analysis of Chiropractic Care and Cervical Artery Dissection: No Evidence for Causation. Cureus.
2016;8:e498.
18. Kosloff TM, Elton D, Tao J, Bannister WM. Chiropractic care and the risk of vertebrobasilar stroke:
results of a case-control study in U.S. commercial and Medicare Advantage populations. Chiropr
Man Therap. 2015;23:19.
19. Cassidy JD, Boyle E, Cote P, He Y, Hogg-Johnson S, Silver FL, et al. Risk of vertebrobasilar stroke
and chiropractic care: results of a population-based case-control and case-crossover study. Spine.
2008;33:S176-S183.
20. Hebert JJ, Stomski NJ, French SD, Rubinstein SM. Serious Adverse Events and Spinal Manipulative
Therapy of the Low Back Region: A Systematic Review of Cases. J Manipulative Physiol Ther.
2015;38:677-691.
21. Dagenais S, Brady O, Haldeman S, Manga P. A systematic review comparing the costs of
chiropractic care to other interventions for spine pain in the United States. BMC Health Serv Res.
2015;15:474.
22. Goertz CM, Long CR, Hondras MA, Petri R, Delgado R, Lawrence DJ, et al. Adding chiropractic
manipulative therapy to standard medical care for patients with acute low back pain: results of a
pragmatic randomized comparative effectiveness study. Spine (Phila Pa 1976). 2013;38:627-634.
23. Hertzman-Miller RP, Morgenstern H, Hurwitz EL, Yu F, Adams AH, Harber P, et al. Comparing the
satisfaction of low back pain patients randomized to receive medical or chiropractic care: results
from the UCLA low-back pain study. Am J Public Health. 2002;92:1628-1633.
24. Carey TS, Garrett J, Jackman A, McLaughlin C, Fryer J, Smucker DR. The outcomes and costs of care
for acute low back pain among patients seen by primary care practitioners, chiropractors, and
orthopedic surgeons. The North Carolina Back Pain Project. N Engl J Med. 1995;333:913-917.
25. Kane RL, Olsen D, Leymaster C, Woolley FR, Fisher FD. Manipulating the patient. A comparison of
the effectiveness of physician and chiropractor care. Lancet. 1974;1:1333-1336.
26. Hurwitz EL. The relative impact of chiropractic vs. medical management of low back pain on health
status in a multispecialty group practice. J Manipulative Physiol Ther. 1994;17:74-82.
Thanks for such a detailed reply Diane.
To me it looks like we agree on quite a bit. We both agree that traditional chiropractic treatment is lacking in evidence. We both prefer conservative, lifestyle approaches to medication and surgery where possible. And we both refer to high quality evidence to support our arguments. This is very encouraging!
We both agree that spinal manipulation may be appropriate for neck and back pain. I’ll have a look through the relevant references you’ve provided, and will update my comments about this if warranted. As this isn’t my area of expertise, I will be guided by the consensus of systematic reviews.
Again though, I don’t make a direct comparison of the education of medical doctors and chiropractors. My interest is in the biases, and errors in knowledge, of chiropractic students and graduates. And regardless of how many hours someone has spent in training, if their knowledge is flawed, we need to question the quality of this training.
Hopefully, Dr. Smith’s got you to rethink your position that comes across biased in my view. Rare is the person that will not defend their position. I hope you are rare.
On another note, being a Chiropractor can be compared to living in the south as a black man during Jim Crow laws. Any Chiropractor that has been around for a while could tell you of stories of being ostracized, belittled looked down upon. In the early days of Chiropractic in order to get a license in a particular state the new DC would have to be willing to get arrested. Many were willing. Some of their views may seem extreme today but without them being that committed Chiropractic may not have survived. The stories we could tell about discriminations might surprise you. Despite the most resistance of probably any profession in the world Chiropractic grew in popularity. Stop and ask yourself why that might be. The answer is simple, a person would seek out a Chiropractor because nothing else would work. That does not make Chiropractic better than any other profession its just that we fill a particular niche in a unique and effective way.
Interesting to me that Physical Therapists (Who I respect and appreciate) have long apposed Chiropractic but are now offering doctoral programs and spinal manipulation. I suppose copying is the best compliment one could pay.
Despite the flawed people like myself that make up this profession it will continue to grow. I’m grateful for the resistance because it refines us and unites us. Blessings to you!
Hi Gregory, my position is informed by research, and my sources have been provided. You are welcome to examine these sources and let me know what I’ve misinterpreted. I will gladly update my article if I’ve made an error, and have done so in the past. A brief history of edits is provided at the end of the article.
I would imagine that your comment that “being a Chiropractor can be compared to living in the south as a black man during Jim Crow laws” will be highly offensive to some people. Criticism, even ostracism and ridicule, is not the same as lynching, don’t you think?
Just curious if you have done a similar review of the education MDs receive? I feel a much more scathing review could be made of MDs as a whole including the biases they have and the harms they are responsible for in their patients health including and not limited to death. Someone once told me this when comparing themselves to other mechanics in my area and it stuck with me ever since, it goes as follows; “it only takes a C to pass a class, very few students are A+ And top of their class. Whether they are a mechanic, nurse, lawyer, or doctor the fact remains that a majority of anyone in their profession is average at it compared to the whole, and unfortunately very few individuals are remarkable at their job.” I make this point because I think too often people (such as yourself in this article) don’t mind painting a whole profession with such a broad stroke of skeptism or even sensationalism, to the point of making a mockery of the entire profession and those who are part of it either as a professional or patient. Which is odd because you yourself can attest to the fact that there are good chiropractors, arguably even great ones. People who are sought after by nurses and doctors themselves, because when you’ve gone to a great chiropractor you know it. Your body tells you with how amazing you feel as evidence by both the research and personal testimonials of people even in this very thread. I’ve personal worked for a chiropractor for two years and can attest to the fact that 100s of their patients would go on record saying how much their overall health and well-being has improved since seeing said Chiropractor. Honestly that job changed my life. Both physically from seeing the chiropractor myself, but also mentally getting to witness time after time patients entire demeanor change as they entered; someone who was in terrible pain and literally at their wits end because their doctor is saying they will need surgery, to six months later walking in standing tall with a huge smile exclaiming to everyone in the office that they threw their last bottle of pills away last night because they no longer needed their pain medication. That is a true story I witnessed and it’s only one of many. I loved that job so much because everyday the entire office was so electric, the energy in their was amazing because unlike a typical doctors office everyone was leaving feeling better and thus happier then when they got there. It was infectious almost and the patients loved sharing their own stories about how/why they came in, and how far they’ve come, it was quite an inspiring place to work. Sorry I got little sidetracked there with the personal anecdote but I feel it’s valid to the argument. To your points, yes you’ve made clear and valid points, love the research as well and your willingness to respond to others in this thread. If possible and for context, I would like to ask you or anyone whose received care from both a great chiropractor and a great MD alike. Would you rather place your trust in the advice of a top chiropractor or a top MD? Personally I would choose a Chiropractor, as they have more training in almost every discipline studied by medical doctors as proven above in a previous comment, plus my own personal experience. The reason I ask is because I’ve heard so many amazing reviews and personal accounts of people’s lives being changed by a Chiropractor, but I can’t say I’ve heard the same raving reviews for MDs.
Thanks for such a thoughtful comment Kyle. It’s hard for me to respond to anecdotes, but it’s great that you had such a good experience. And of course, there are good and bad in every profession.
In answer to your first point, I haven’t done a review of the education of MDs, as that’s a little out of my field. But I have written articles about physiotherapists and personal trainers on this site, and have been highly critical of both when it is deserved.
This is an excellent article. I worked in P.T. As an assistant for many years and saw many patients with really bad injuries from their Chiropractor. Glad you wrote this article. People are often trusting without examining the consequences of seeing someone who is not a medical doctor. I am retired and notice that people are very defensive when you care enough to give an educated opinion. Thanks for your work. Take care, Hillary Wolf
Thank you for commenting Hillary! Yes, the response to criticism has been a little surprising. In academia we see thoughtful, informed criticism as an opportunity to improve.
“Johns Hopkins study suggests medical errors are third-leading cause of death in U.S.”
https://hub.jhu.edu/2016/05/03/medical-errors-third-leading-cause-of-death/
Allopathic medicine, in general, is from being without risks.
And, anecdotally, as a chiropractor of 10 years, I’ve treated many people injured by their PT and injured by other DCs so I’m not sure what your point is. Any and all intervention is not without risks.
I’ve also treated people injured while lifting their children, while driving their car, while walking or running, from sleeping, from bending, from sneezing…and a whole host of other mechanisms of injuries.
I have never considered going to a chiropractor, not because I dislike them but because there is no need. If you ask me if I trusted them I’d give 5 out of 10. But just before the lockdown last year I experienced a nagging pain around my neck and shoulder. It was not acute pain but a dull pain that simply won’t go away. It lingered for a month and each morning I dread waking up. My neck was stiff and sore, I couldn’t turn normally. In a mall one day I just happened to walk pass a chiropractor. It was giving a one-time promotion and out of desperation I decided to go in. I didn’t actually believe it would work. Cut long story short, he examined me, pressed here and there, asked a few questions and then he twisted my neck. I was shocked at the cracking sound. He did it a second time in the other direction. I couldn’t believe how loud it sounded, my bones. But when I stood up the pain was gone. Like magic. Till today I am pain-free. I have never gone back to see the chiropractor. But he really helped me. I wouldn’t mind giving him a hug for what he did. So although I still have my own reservations, if desperate, I would try it and do it again.
It’s great that you had a positive experience Larry, that kind of pain can be really horrible!
I feel I must defend my chiropractor. After a car accident, I became unable to turn my head to the left for perhaps 2 years. After my first visit, my neck fully released and I had full range of motion.
My husband saw the same doctor for acute lower back pain that was level 10 for a few days and the pain could not be controlled w/ heavy medication. (PCP had said well if he’s not better in a week I’ll order an MRI and that was all he could do!). After the first
visit to the aforementioned chiropractor his pain was immediately reduced to a 3.
I’m glad you and your husband had good experiences Theresa. As I mention in the article, there are some great chiropractors out there, doing wonderful jobs within their scope of practice!
I’ve been licensed practicing chiropractor for 33 years here in PA. Grew a family, put the children through college, paid all my bills and have had a wonderful life. Great rewarding profession. I’ve seen quite a bit of health care providers who can’t say the same and are actually in jail for fraud. What qualifications and experience do you exactly have.
Thanks for commenting Mark. As I mention in the article there are many great chiropractors out there, of which I’m sure you are one. But that is a different issue to the problems with traditional chiropractic practice and education, which was the main point of the article.
As a chiropractor who is leaving the profession in a couple of months, I agree with the majority of what is being said here. I did want to point out a statistic in the “Why Chiropractors” section of your that is being skewed.
In regards to CAD/stroke, you state that “Estimates of how likely this is vary, as these events don’t always occur immediately after the treatment. But we think they occur about once in every 100 000 adjustments…” The study you link states the occurrence of CAD/stroke is between 100,000 – 2,000,000. This paints a very different picture than just using 100,000. It would be a more accurate representation of the data if you used the range.
Thanks for reading Cory, and you’ve made a fair criticism. I’ll check for more recent literature, and then update this sentence.
YOU RAISE SOME GOOD ARGUMENTS. THE PROFESSION NEEDS A MANDITORY PRE ENTRANCE TO GET INTO A CHIROPRACTIC COLLEGE. WE HAVE ONE ITS PRODUCED BY NBCE AND IS CALLED C-CAT. SOME COLLEGES USE IT NONE REQUIRE IT. IM ONE OF THE 6% YOU SPOKE OF. I PRACTICE CHIROPRACTIC ORTHOPEDICS.I HAVE TRAINED FOR IT TO INCLUDE CASE WORK FROM HARVARD MED,MAYO CLINIC AND U-MICHGAN MED.I TREAT PAIN AND DO SO WELL AS MEASURED BY PATIENT RESPONSE.MOST ARE TREATED AND RELEASED IN 8 WEEKS OR SO. I TO DO A VASCULAR SCREENING PRIOR TO MANIPULATION OF THE C-SPINE, ESPECIALLY IN THOSE KNOWN TO BE PRE DISPOSED. I HAVE REFERRED MANY WHO HAVE SHOWEN IMPENDING CAROTID OR VERTEBRAL ARTERY OCLUSSION.AS TO DIAGNOSIS I DO IT. 70 CONDITIONS CAN CAUSE BACK PAIN BESIDES THE BACK. I TREAT WHAT I TREAT AND REFFER WHAT I DONT TREAT AND I KNOW THE DIFFERENCE. MY CLINICS ALL DO THIS AND ALSO PT AND REHAB SERVICES. OH AND YES I EMPLOY MDS AS WELL,AND HAVE DONE SO SINCE 1984. IM 46 YEARS IN THE TRENCHES AND IM SUIT FREE. IN CLOSING I FEEL THE PROFESSION WOULD BENEFIT FROM ADDITIONAL TRAINING AND AN “ADJUSTMENT” OF THEIR PHILOSOPHY.
Thanks for commenting, you sound appropriately cautious and professional, it’s great to hear.
Thanks for this post. Love how you cite scientific studies. I hadn’t realized there were essentially two schools of chiropractic thought (old school vs new school we could call it). What percentage would you say fall into each camp? I can tell which one most of the people responding fall into haha…
Thanks for reading Eileen. In my anecdotal experience supporters of the traditional approach are certainly more vocal! I think one of the papers I link to has an estimate of numbers in each camp, if I find it I’ll include the source and estimate here later.
Hmm. There is One Federal agency in charge of accrediting All Chiropractic schools so this article is incorrect regarding the school’s Philosophy directing the educational requirements. Same with the testing prior to licensure. As for the education, 2 years of cadaver dissection in every Chiropractic school speaks volumes on the extensive education.
Hi Andrew, thanks for commenting. I’ve referenced that claim, so you’re welcome to examine the original research if you would like to know more. Much of this research is written by chiropractic educators, so I find it reasonably compelling.
“Mystical” healing powers within us? There’s nothing mystical, you twit. It’s called science. This article is absolutely a joke, and so, since it’s created or written by you, YOU are a joke. Why not spend your time doing something useful and relevant, you moron. Chiropractic has proven itself since 1895 to be a drug less, safe and completely effective approach to enhancing the recuperative abilities of the body. We never claim to heal anything, you idiot. Only the body itself heals! Duh. Get a real job, butt wipe.
I’m heartened by the fact that you’ve overreacted to a choice of a word, rather than identify any significant flaws in my article. If you do, let me know, and I will gladly make a correction.
Criticism and argument is a cornerstone of science. Consider that when you’d like to call someone else a “butt wipe” when they disagree with you!
Abstract: who wrote this filth. Firstly, you have to talk to the U.S. Department of Education about what a doctoral program is and what isn’t. Second chiropractic education SUPERCEDES any doctor of medicine degree…how do I know? I’m a chiropractor who currently is in a doctor of medicine program and whom is bout to graduate. And trust me you do not get accepted into a medical school being a quack or having not fulfill the requirements. EVERY DOCTOR WHETHER CHIROPRACTOR, PODIATRIST, SURGEON etc has had Organic Chemistry, Microbiology, biology, physics, general chemistry, biochemistry etc…see it. Thirdly, the reason why I went back to obtain and MD was to satisfy my curiosity and to de-mystify the theory that an MDs education is superior to my publicly perceived ” lower shelf quakopractic education”…trust me it’s not. I also wanted to be able to thwart and debunk disgusting, and disingenuous arguments and conjecture like what I just read. This author has probably never sat in any physiology or anatomy dissection ever… not only that…he or she probably doesn’t have a biology/ chemistry degree as well…but I guess biology and chemistry degrees are fraud degrees too. Conclusion: the author is an idiot… by law …by law chiropractors are primary health care providers with national physician identification numbers. It is against the law to promote public distrust against them as well. Watch what you write.
Thanks for reading Tim.
It’s great that you are furthering your education. But part of your impetus for this was “I also wanted to be able to thwart and debunk disgusting, and disingenuous arguments and conjecture like what I just read”. You had an opportunity to do so right here. Instead you chose to hurl insults! I’ve supplied references to supports my “conjecture”, some produced by chiropractors in research positions.
So feel free to read a little more deeply, and if you identify any specific errors I would be glad to correct the piece.
The author of this article is a COWARD first and foremost. Nice job hiding your name.
The world does not need any more poseurs spreading false and misleading information, pretending to be experts just because they own a computer.
You have an extreme and yet naive bias towards the medical profession. Research based(?!) in medicine is laughable. There are countless examples, can your miniscule brain even comprehend OPIOID EPIDEMIC? Is that not what your coveted medical research produces? This has killed 100 times more in the last decade worldwide than all Chiropractic has since its inception.
I hope you get the chance to suffer, as you would have others do, at some point when effective treatment is denied to yourself or a loved one, because some loser like yourself has invalidated it.
Hi Mike, you can find my name, and details of my qualifications and experience, on the “about” page of my website. Hardly hiding, don’t you think?
I didn’t criticise the medical profession in this article, because it wasn’t in the scope of the article. But in other articles, I have criticised other professions. You’re only mad about this one because it challenges a belief that is obviously very important to you. So mad that “you hope I suffer”, apparently. That’s not very nice Mike.
I am an Exercise Physiologist and am currently completing a PHD in TBI and spinal reflexes. I have a sibling who is a chiropractor and has been practising for 10 years. I am amazed on what he advises as medical advice and how much our training differs. He also touts his experience qualifies him for as a personal trainer and delivering exercise prescription for any condition. Another sibling (neurosurgeon) and I often are amazed at how much he doesn’t know about the spine, neurology and physiology, especially in relation to development and and injury. It is not a point we argue because this individual won’t listen. If chiro’s were a little more like every other medical and allied health professional and said “we don’t know but I will find out” rather than believing their training has ALL the answers they would do a lot better.
Great comment, thank you. Appreciating the limits of your expertise is not something that every professional has a great grasp on, unfortunately, even in more evidence-based professions.
In your very first paragraph you state that “Estimates of how likely this is vary from once in every 100 000 to two million adjustments, as these events don’t always occur immediately after the treatment. They result in death in 18% of cases.”
You then link to a PubMed article which clearly states “Results for those aged /=3 visits with a cervical diagnosis in the month before the case’s VBA date (95% CI from bootstrapping, 1.34 to 18.57). No significant associations were found for those aged >/=45 years” which is nowhere even remotely close to 18%. Even the research paper itself states “While our analysis is consistent with a positive association in young adults, potential sources of bias are also discussed. The rarity of VBAs makes this association difficult to study despite high volumes of chiropractic treatment.”
While the risk of VBA dissection is possible, it is extremely low, and always has been. As mentioned by others, malpractice insurance rates for chiropractors is exceedingly low because the risk of adverse events like death are so rare. Insurance companies are not stupid; they don’t make poor bets. Please don’t use statistics if you are uneducated in their application and significance. And do not fabricate numbers just for your page.
Hi Benjamin, thanks for reading. I’m not sure how the quote you’ve pulled contradicts me though. You are referring to the total number of injuries, and I’m referring to the deaths from these injuries. Obviously these are different things, wouldn’t you agree? The 18% number is actually from the full text of the paper I linked to, and not the abstract, which is where you pulled your quote from. I’d always suggest reading the full paper rather than just the abstract, particularly when you are going to accuse someone of being uneducated and fabricating numbers…
So I’m comfortable with the statistics I’ve cited.
I have made one mistake when I went back to check my sources, just not the one you think I did. That is not citing the original source for that statistic, but rather a secondary source. The paper I linked to was citing earlier research which reviewed case reports of this type of injury. The identified 29 deaths from 165 cases in the literature to that date, or 17.6%. I’ve updated the link so it refers to the original source.
Wow, I can’t read anymore comments.
I feel like practitioners failed to read the article almost at all, and were bias from the start based on the title. Which is a shame.
Of the comments I did read, it doesn’t seem like they really picked up on you saying that you’ve had good experiences with chiropractors yourself. I took your article as new information to consider, not as advice that I shouldn’t consider chiropractors as an option for treatment.
That so many practitioners took your article as an attack on them (almost personally) speaks volumes about their awareness of the flaws in their education. But why they’re inclined to not consider what you’ve said at all, instead of taking insult, is beyond me.
The information you’ve provided in the article is almost outshined by the information I gained from reading their comments claiming you’re a hack writer paid by some competing medical practice. All without supporting their claims with any new information too be referenced.
Which is comical, since we know that roughly half of what medical professionals are taught in school will be proven wrong in the 2 or 3 decades afterwards.
Thanks for the information, I love your response to all of the people with no supporting evidence to their claims.
Thanks for reading Erik! Their responses are very informative, aren’t they? It’s beyond me too… I can’t imagine other professions reacting this way to evidence-based criticism.
First off i’m not a chiro, however i like to read justified pieces.
This seems to be an extremely simplistic approach to belittle chiropractic.
Yes, there are issues, as they are with nurses playing gp’s or physio’s playing with manual therapy ?
I think the biggest misconception of chiropractic, is that performing hvla spinal manipulation is difficult, usually only people that are sporty can combine the skillset.
Hence, the majority cannot express themselves very articulately and come across as idiots.
Would i visit a chiro ? Not sure.
Are they undereducated?
5 years at a government funded uni is definitely a long commitment and i dont believe that go there to high five each other.
Are they as educated as medical doctors ?
Depends , on musculoskeletal issues and diagnosis i believe they eat a gp for breakfast, on other issues no.
Are they better trained than physios?
Yes ,.
Should they improve?
Yes
Well, there’s at least one thing we agree on Don, a lot of the chiropractors that comment on this article are certainly not articulate!
Back in 2006 i went to a chiropractor [edited] who sadly in is 70 still practice and is a real danger he is now based in Connecticut.
I went to is practice with lower back pain, he over adjusted me and left me after 6 months in terrible pain, now i had neck and middle back pain snapping ribs, snapping hips and pain in one side of my hip and my lower back pelvic was getting worse. Yet he still believed in chiropractic being a cure all and wanted to continue the treatment, when i confronted him is attitude changed and he sent me to another chiropractor.
Chiropractic is very dangerous don’t ever believe the chiros that come on here and say it saves lives its hypocrisy at its best.
A chiro told me that i had subluxation cause my muscle spasm and he was the only one able to cure me so every week he adjusted me never knowing that i had ligament laxity made worse by is adjustments.
I met a few of [edited] old patient that he got worse and this guy always got away with it he is now online even giving diet advice and more and yet he is a chiro with no dietician baseline.
Never ever go into a chiropractic clinic you will come out worse then you got in.
Sorry you had such a negative experience Yannick, I’m glad you’re feeling better now
I’ve edited your comment to remove the names of specific practitioners, and recommendations for specific treatments. But as always, I would encourage readers to seek advice from appropriately qualified professionals. And if you aren’t sure about the treatment or advice you receive from one professional, promptly seek a second opinion.
I enjoyed this article. I suffer presently (less than 12 days) from Sciatica. I’ve seen as modern, open-minded Chiro as one could hope for. His adjustments provide only transitory relief (hours) but after day ‘one,’ when pain was most intense, this was much better than ‘nothing.’
I wanted to ask about PT’s as your statement somewhere in this fine blog mentioned you’re being critical of them at some points in time.. My experience with them has been negative – however, this has NOTHING to do with their efficacy vs. chiropractors. Just personal experience. Mine has been, probably by coincidence, that the PT’s said seemingly crazy things. Also, their exercises including using a balloon, were so complicated I simply could not do them without help. One, a great guy who may be completely correct!…told me my gait was sideways, probably from a catastrophic football injury – which I informed him of. As I was referred to him by my M.D., I’m curious if the doctor knows this guy was making such bold statements. Again – he may be correct.
Q. What was some of the basis for your criticism of PT’s? Very curious. Also, if the Sciatica doesn’t resolve itself as I hope, given my experiences, I’m leery of seeing another PT.
Thank you.
Thanks for reading Allan.
I think like all professions, there are good and bad examples among practitioners. So as you brilliantly identify, we always need to be cautious that our experience may not be typical. My criticism of physiotherapists has also been informed by research, and I’ve provided the link to the article below. Based on the numbers I’ve seen in the research, you can be more confident that a physiotherapist will be providing evidence-based advice. But it sounds like you met an interesting one!
https://criticalfitness.com.au/physiotherapists-provide-evidence-based-treatment/
I appreciated your article. I am an Australian chiropractor with 46 years in practice currently undertaking a PhD. I wonder how many of the objectors to your article have read DD Palmer’s only published book ‘The Science Art and Philosophy of Chiropractic. I have read the 1,007 pages of that publication.
In my opinion no intelligent reader could read that book and still believe Palmer’s theories like ‘innate intelligence’ were logical. I have studied the Palmer for many years and have read everything DD Palmer wrote that is currently available. He was a typical 19th century ‘health’ entrepreneur of the same ilk as AT Still, who did not have one original idea of his own. The ‘subluxation’ concept credited to Palmer did not originate with him. Harrison used the term/concept extensively in 1827.
I suggest most chiropractors would be unaware that Palmer claimed he was ‘curing’ ‘disease’ states such as hemiplegia as early as 1888. That is is 7 years prior to the amazing discovery of chiropractic which was given to him by a spirit from the ‘other world’. I wonder if any chiropractors can explain how or why DD Palmer died from two disease states that he claimed could be cured by chiropractic i.e. typhoid fever & brain congestion. These are listed on his death certificate. I have a copy of the original certificate. Also, why did BJ Palmer (DD’s son & heir to chiropractic) die from stomach cancer if chiropractic can cure cancer as DD & BJ claimed?
Thanks for reading Desmond, I appreciate the background you provide here! I have no intention of reading Palmer’s book, so I also appreciate that you endured it for me!